Diabetic Retinopathy
A concern for all diabetic patients, specially after the diabetes has been present for 8 or more years, is the development of blood vessel instability within the retina, a condition which is known as diabetic retinopathy. There are two types.
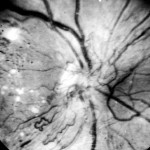
Background Diabetic Retinopathy
Background diabetic retinopathy occurs in middle or older individuals and is the more common type. See below on the left. The retinal capillaries become excessively permeable, and the retina becomes swollen, or boggy. The excessive leakage is the result of focal dilation, or microaneurysms, having developed within the capillary system. The location of the microaneurysms is made possible by a photographic circulation study known as fluorescein angiography. Click on photos to enlarge.


When the background retinopathy begins to threaten visual function, by encroachment on the macular retina, laser coagulation becomes necessary. For that procedure a 50 micra light is precisely directed at the microaneurysms, the identification of which has been aided by fluorescein angiography. Equally important is maintenance to a 500-750 mg sodium restricted diet.
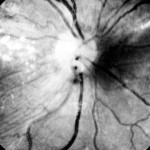
For some diabetic patients the background retinopathy can become quite severe in a short period of time. Factors that can contribute to such a development in more or less degree, are (1) decreased kidney function, (2) elevated blood pressure, (3) fluid retention, (4) congestive heart failure, and (5) cataract surgery. The latter is reasonably well tolerated for most diabetic patients, but for some the diabetic retinopathy can destabilize following the surgery. Diabetic retinopathy with severe congestion might require anti-VEGF or corticosteroid injection as well as vitrectomy with removal of all vitreous attachment to the retina.
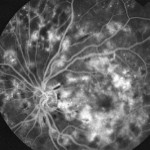

Proliferative (hemorrhagic) Diabetic Retinopathy
Proliferative (hemorrhagic) diabetic retinopathy is more likely to develop in the younger diabetic or in the older diabetic as a late complication. The term proliferative refers to new blood vessel fermation. The new blood vessels are poorly developed and inclined to rupture. See below. Hemorrhage within the vitreous cavity is the likely consequence of the neovascular phenomenon. Scarring within the vitreous is another likely development and following that development, retinal detachment is likely. See below.
Proliferative diabetic retinopathy requires ablative laser coagulation to the neovascular blood vessels and also to retinal sites that are receiving a poor blood supply. It is thought that the new blood vessel growth is nature’s attempt to provided greater blood infusion to the retina; in this particular situation, though, the neovascularization does not penetrate the retina and, therefore, serves no useful purpose.
If the bleeding cannot be controlled by laser coagulation, an operation procedure, termed vitrectomy, is necessary to remove the blood and scar tissue that might have resulted therefore.


Low Sodium Diet
Low sodium diet is an important component of the measures that are necessary to obtain the best control of diabetic retinopathy. For most patients laser coagulation and low sodium dietary measures provide a good result: reversal of the retinopathy and improved visual function. The low sodium diet reduces the number of laser coagulations that are required. Sometimes additional measures are required to obtain a good result, but laser therapy and a low sodium diet are the cornerstones for a good result.