Macular Degeneration
Degeneration of the macula, the central retina responsible for detail vision, is the leading cause of visual disability for the elderly. At sixty-five years of age approximately 2% of people have some degree of central retina deterioration, as clinical studies have shown. At seventy-five, the incidence increases to 11%. By eight-five, the incidence escalates to 27%.
Macular degeneration occurs with greatest frequency in blue-eyed Caucasians. It is an unusual cause of visual loss in blacks.
Dry-type Macular Degeneration
Drusen
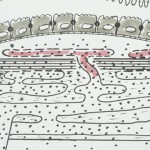
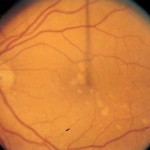
The breakdown area is a deep collagen membrane (Bruch’s) that lies between the retina and a posterior blood vessel layer known as the choroid. Within increasing age Bruch’s membrane loses its ability to control the diffusion of serum into the retina. As a result discrete and slightly elevated fluid precipitates known as drusen from beneath the retina. (see below, left). Click on photos to enlarge.

Low Sodium Diet
Macular degeneration occurs more commonly in individuals who consume 3000 or more mg of sodium per day. Sodium in that amount causes an abnormally elevated filtration pressure across the collagen membrane that can be tolerated by some eyes but not by others. The cause for macular degeneration requires abstinance from dietary salt and high-sodium processed foods. That regiment was effective for the patient whose left eye was shown above. Note approved appreance following 28 months adherence to a 750 mg low sodium diet.


Shown below are two other examples of drusen regression following a low sodium diet. Sometimes 36-42 months adherence is necessary before regression is complete for the macular retina. Click on photos to enlarge.
If sodium restricted dietary intervention is not undertaken, drusen ultimately cause atrophy/death of contiguous retinal cells. The result is extensive degeneration within the central retina and a profound loss of central vision function. See an example of advanced dry-type macular degeneration that followed regression of long-standing drusen.


Wet-Stage Macular Degeneration
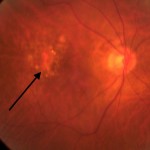
Blood vessel proliferation through the a weakened Bruch’s membrane is a feared complication of the macular degeneration process. The blood vessels are poorly formed and they are susceptible to break-down with bleeding. An example of hemorrhagic (wet-stage) macular degeneration is shown below. Click images to enlarge.

Treatment
Wet-stage macular degeneration is managed with a medication that is injected into the vitreous through the wall of the eye. The medication, anti-VEGF (anti-vascular endothelial growth factor), diffuses posteriorly to the macular retina and the blood vessels which have caused bleeding. The medication has the effect of attenuating (narrowing) the abnormal vessels and controlling the bleeding. Oftentimes, the injection must be repeated several times over a many month process. Treatment of such type consistently provides resolution of the wet stage process and, for 40% or so, a modicum of visual improvement.
Both dry and wet stage macular degeneration require an appropriate amount of concern and attention by both the patient and the retinal specialist. To not do so could result in irreversible damage and visual impairment.